
Starting out on a low FODMAP diet can be bewildering – and even more so if you’re following a plant-based lifestyle. In this post, I share be key lessons I have learned on how to follow a low FODMAP vegan diet and get my symptoms well and truly under control. Yay!
Adopting a new way of eating can be daunting and a little overwhelming, and I coped with this by simplifying – distilling the information about a low FODMAP vegan diet down to just six basic rules: eat lots of low-FODMAP greens for bulk and fibre, add low-FODMAP protein, avoid feeling deprived by baking with erythritol/stevia sweetener and gluten-free flours, go easy on fruit, space your meals, and focus on keeping yourself in a relaxed frame of mind as much as possible.
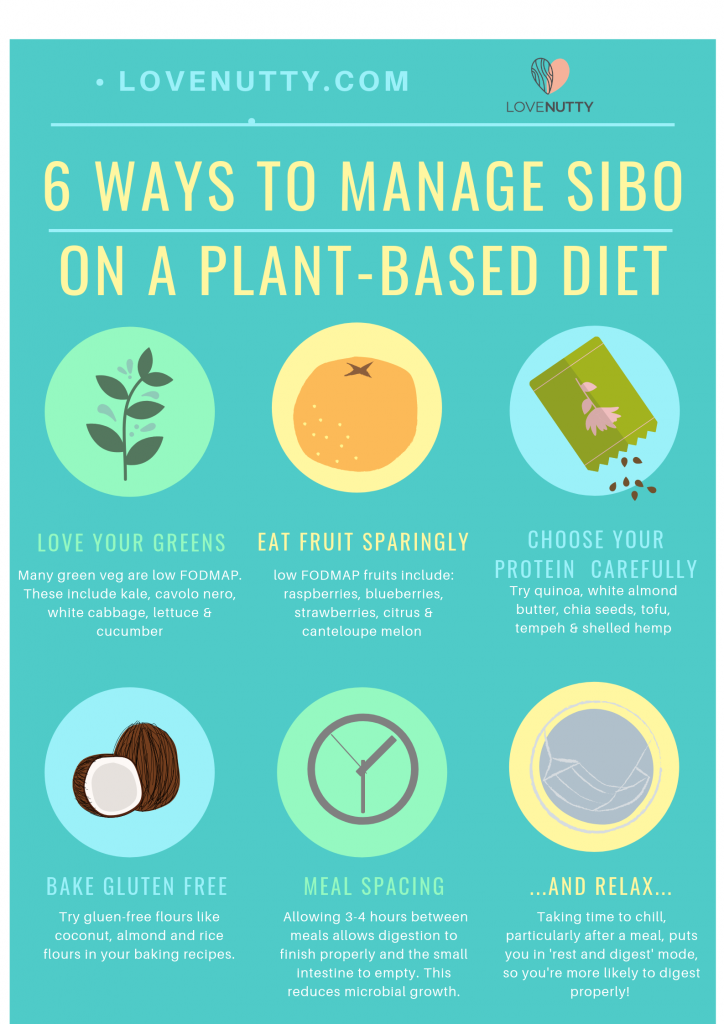
Managing IBS or SIBO on a plant-based diet
Digestive issues like small intestinal bacterial overgrowth (SIBO) and small intestinal yeast overgrowth (SIYO) are challenging – and ever more so if you are following a plant-based diet where usual sources of protein like legumes are out of the question. Personally, I find I cant even tolerate brown lentils, whcih are supposed to be low FOSDMAP. We each have to find our own set of tolerable foods, it seems, depending on our individual complement of troublesome microbes.
Many of us have tried endless diets and expensive supplements only to find that ‘permanent cure’ seems out of reach.
Symptoms improve for a while, but sure enough, after a few weeks or months, the old problems return and we’re back to square one. Find out why this is pretty much inevitable if you’ve had SIBO for a while in my post about biofilms, which also covers tactics for getting rid of the biofilms in your gut for longer lasting improvments in health.
What is a low-FODMAP diet?
‘FODMAP’ stands for fermentable oligosaccharides, monosaccharides and polyols – basically a group of short-chain carbohydrates that are not absorbed by the gut and are instead fermented by your gut microbes.
If your digestive problems are linked to dysbiosis (imbalance of microbes) then eating low FODMAP foods is likely to ease your symptoms.
Ideally this would be combined with supplements that break down biofilms (see my post on biofilms) and broad spectrum probiotics.
Caveat: long-term low FODMAP diet needs to be carefully managed
What isnt mentioned in most articles about a low FODMAP diet is that it was never designed for long term use. Even the researchers at Monash University who developed the diet say that it is designed to be followed for “2-6 week period of high restriction and then transitions to a more relaxed diet where certain foods are gradually re-introduced” [source].
A down-side of a long-term low FODMAP diet?
The reason for the recommended short duration of severe FODMAP restriction is because these particular carbs are important for keeping your large intestinal microbiota happy – and this is crucial for health! By starving your SIBO of its favourite food to control your symptoms, you’re also starving the microbes you do want to feed – in your large intestine.
A low FODMAP diet – with its reduced fermentable fibre can have a similar effect on your microbiota and colon heath as a junk-food diet – which is also low in fibre. There is evidence that a diet low in fermentable fibres can cause inflammation in your large intestine [source].
And a solution!
In my personal experience, the solution is to eat a low-and-occasionally-moderate FODMAP diet, and tons of low-fodmap greens. This provides non-fermentable fibre and nutrients to maximise gut – and body – health, while mostly controlling symptoms. Try it – it might work for you!
Take the pressure off…
In the meantime, however, what we can do is to take the pressure off ourselves, accept where we are at the moment and focus on long-term symptom management with things like a low FODMAP diet. It can be done! Now, doesn’t that feel better?
And…relax (with a cup of peppermint tea) and read on…
1. Low FODMAP vegan diet tip: Learn to love your (low FODMAP) greens

Eating low FODMAP vegan diet means cutting down the soluble, fermentable carbs in your diet. To compensate – and minimize the deleterious health consequences of long term reduction in fermentable fibres – I suggest eating lots (as many as you can tolerate) of insoluble/non-fermenting carbs and fibre.
If you are in a full blown SIBO attack, then you might need to wait for that to calm down (white rice and low-FODMAP protein can work here – see my blog post). But in terms of long-term management, loving your greens will help to ‘keep you regular’ while minimizing bloating and other symptoms.
symptoms.
| LOW FODMAP GREENS | HOW TO PREPARE/COOK |
| Kale | Remove any large stalks. Chop finely and steam or saute in a little coconut oil |
| Cavolo nero | Strip the leaves from the stalks. Chop finely and steam or saute gently in coconut oil or extra virgin olive oil |
| White Cabbage | Slice into thin strips and saute gently in cocounut oil until browned and crispy. |
| Salad leaves | Most salad leaves are low-FODMAP. Serve with plant-based protein and a great salad dressing (and chew well!) |
| Cucumber | Fresh and cooling, this wonderful fruit can be used in juices or salads. |
2. Low FODMAP vegan diet tip: Eat fruit sparingly

Keeping your sugar intake low is a good idea generally, but if you have SIYO or SIBO, it is particularly important. The small intestinal inflammation that comes with these conditions can means that we are not able to process fructose as efficiently, and this can encourage SIYO and SIBO. For more information on why this is, check out siboinfo.com.
Fruits with an excess of fructose (i.e. the glucose content is higher than the fructose content) will cause the most problems.
Remembering the list of lower fructose fruits can be tricky. As a rough guide, stick to:
- berries
- cherries
- citrus
- kiwi
- canteloupe
Low FODMAP vegan Blueberry & coconut granola pot

[ingredients title=”Ingredients”]
- 1/4 cup blueberries
- 1/4 cup coconut yoghurt
- 2 tbsp LOVENUTTY Granola No. 2
- 1 tbsp pomegranate seeds
[/ingredients]
[directions title=”Directions”]
- Wash the bluberries and place at the bottom of a glass.
- Layer on the coconut yoghurt – I use the thick type that is higher in fat so more satiating
- Layer on the granola and top with the pomegranate seeds.
- Serve with a cup of green tea for a light and gut-healthy breakfast.
[/directions]
3. Low FODMAP vegan diet tip: choose your low FODMAP plant-based protein source carefully
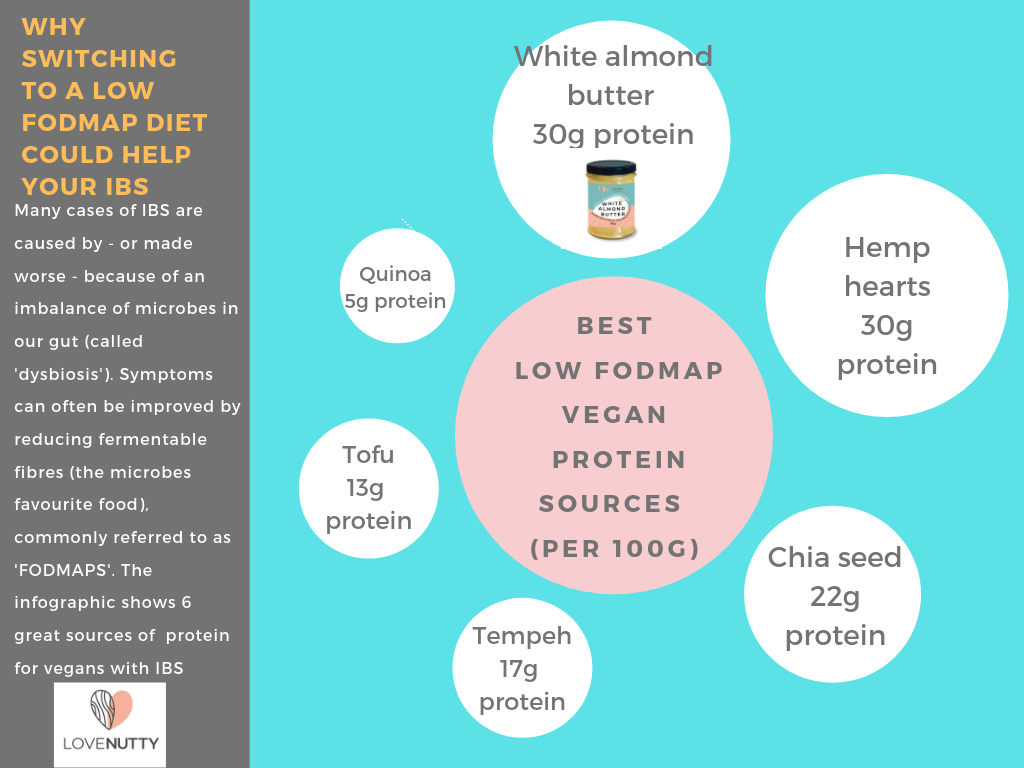
If your following a plant based diet, then the most obvious way to include protein in your diet is to eat legumes and lentils.
But if you have SIBO, these foods can make you feel worse and substantially worsen your symptoms. Luckily there are a variety of other plant-based sources of low FODMAP protein. These are:
- hemp hearts
- tofu
- tempeh
- white almond butter
- chia seeds
- quinoa.
Read more about this in my BEST LOW FODMAP VEGAN PROTEIN SOURCES blog post.
4. Low FODMAP vegan diet tip: Bake using low FODMAP gluten-free flours and erythritol/stevia-based sweeteners

Following a low FODMAP vegan diet means cutting down on sugar, and with this goes so many of our favourite ‘treaty’ foods.
But all is not lost! Switching your baking ingredients to low FODMAP gluten free flours and erythritol-based sweeteners allows to to reclaim the cake..
Why gluten free flours?
Flours that contain gluten also usually contain FODMAPs. Also, the proteins in gluten have been shown to make leaky gut worse. Given that leaky gut is a common problem in SIBO becuase of the local inflammation of the small intestinal lining, it’s advisable to avoid wheat, barley and rye.
- Coconut flour
- Almond flour
- White rice flour
- Hazenut flour
Why erythritol-based sweeteners?
Erythritol is a plant-based sweetener that has zero calories and it’s my favourite sweetener! Why? As it passes through your digestive system, 80% is absorbed into your bloodstream (without affecting blood sugar! Hurray!) and is excreted unchanged by the body; with xylitol, by contrast, all of it stays in the gut, is fermented by gut microbes, hence the diarrhoea and bloating this sweetener causes.
Only 20% of erythritol is left in the gut, and this means very few problems for people with SIBO or IBS. Find out more here.
What about stevia?
Stevia or more accurately, steviol glycosides, are plant extracts of the Stevia plant that grows in to Paraguay and other tropical areas of the Americas. The extreme sweetness of the leaves has been known locally for centuries but has recently been cultivated and manufactured commercially on a large enough scale to be sold in supermarkets. It has a bit of an aftertaste, which some people seem to taste more strongly than others. We only use a very small amount of stevia in our recipes, so the aftertaste is minimal.
As the negatives of the traditional sweeteners (aspartame, Ace-K, saccharin) have been revealed, I think erythritol and stevia together are the most gut friendly and least problematic of the sweeteners currently available.
At LOVENUTTY, We use erythritol and stevia as sweeteners because these have the lowest effect on people with gut issues and are less likely to cause bloating than other sweeteners.
There are thousands of delicious and easy low FODMAP vegan recipes on the internet, including on this site. Perhaps try Salted Caramel Chocolate Brownie, and substitute the recommended 300g of sugar with 220g erythrtitol-stevia based sweetener, or for an even tastier brownie, a ‘brown sugar’ erythritol-based sweetener.
5. Meal spacing: leave 3-4h between meals

In a normally functioning digestive system, around 2-3 hours after a meal, a strong cleansing wave (like powerful peristalsis) sweeps through the small intestine, clearing out all contents into the large intestine. This cleansing wave is technically known as the migrating motor complex (MMC). when your tummy rumbles when you havent eaten for a while -that’s your MMC.
When the MMC doesnt work correctly, the small intestine isn’t cleaned properly and microbes start to overgrow – that is, SIBO.
So no snacking?
Nope. Sorry…
If you have SIBO or sluggish digestion generally, then giving your small intestine its best chance of cleaning itslelf crucial to symptom management.
This means resisting snacking – and drinking only tea or water between meals. If your stomach senses any ‘food’ (even liquid food), it will prevent the MMC from happening, and you might have to wait several more hours to get another MMC!
Larger gaps between meals means less food for the SIBO to feed on, and fewer or less severe symptoms. Definitely a good thing!
What about intermittent fasting?
Another approach that I use often is to skip breakfast and not eat anything until noon – it’s my version of intermittent fasting. I dont do it every day, but I do it most days and it gives my digestion a proper rest and helps to starve out those pesky microbes and reduce their numbers. When I do this regularly, I am much less prone to bloating and other SIBO/IBS symptoms.
6. Relax, rest and digest

It’s hard to overemphasise the importance of relaxing – not just for people following a low-FODMAP vegan diet – but anyone with digestive issues. This is a lesson I have had to learn because my natural (permanent) state is ‘busy-busy’, and this was really not helping. The key to this, it seems, goes back to our school biology lessons.
Remember the ‘sympathetic and parasympathetic nervous systems’? No? Well here’s a refresher: these two systems are like two sides of a see-saw. If you are stressed, the balance will tip towards ‘sympathetic’ – that is, adrenaline, cortisol, ‘fight or flight’. In this state, energy and focus is diverted away from your digestion to your muscles and other relevant areas. Yes! If you’re stressed, you’re not going to be digesting as effectively.
Parasympathetic = better digestion!
‘Parasympathetic’ is the rest and digest mode. This is the ideal state as it is one where we are more calm, think more clearly and work more efficiently (and who doesnt want that!?). We should be in this state most of the time and only call on ‘symapathetic’ when we need to do someting under pressure – but many of us are in ‘sympathetic mode’ most of the time!
I have found that staying in ‘parasympathetic mode’ needs constant attention and vigilance as it doesnt come naturally. I have found I need to consciously scan my body and relax my shoulders, and repeatedly tell myself: it’s OK, everything will get done, there is no need to rush or stress. Everythig is good. I am calm, serene… (you get the picture).
So there you go. My six top tips for managing SIBO – I hope they work for you!

Hi!
I’m Dr Sian and I LOVE experimenting in the kitchen with plants and I am so happy to be able to share my recipes with you here. I live in Wiltshire, UK with my partner and two children.
I post new recipes and articles about heath (particularly gut health) regularly – watch this space! xx

